71 Days in the NICU: How Estelle Overcame PPHN, Endocrine Challenges with Lifesaving Care
- Category: Patient Stories, Neonatal ICU
- Posted on:

For Emily and JD Dunaway, growing their family has been a journey marked by both heartbreak and hope. After two miscarriages following the birth of their first daughter, the couple had paused trying to conceive again—until they found themselves unexpectedly pregnant with their second daughter, Estelle.
“We were so excited,” Emily shared. “It was unexpected, and very sweet.”
Emily’s pregnancy progressed smoothly. “It went really well—I didn’t have any morning sickness, just some fatigue,” Emily recalled. “All of my baby’s ultrasound appointments were normal."
With no sign of complications, the Dunaways eagerly awaited Estelle’s arrival. She was born on her due date—July 23, 2024—at St. Tammany Hospital on the North Shore in Louisiana, weighing a healthy 7 pounds, 1 ounce. But what should have been a joyous moment quickly turned into a critical situation.
“Estelle didn’t cry after she was delivered,” Emily recalled. “She made a few noises, and I was able to hold her for maybe a minute or two before she was taken to the nursery.”
At first, she didn’t look blue or severely distressed, but something was off. Her breathing was shallow and irregular. Even with oxygen, her levels stayed unstable, and she wasn’t improving as expected.
After two days in the neonatal intensive care unit (NICU), doctors ordered an echocardiogram that revealed the cause: Persistent Pulmonary Hypertension of the Newborn (PPHN).
Understanding PPHN: A Life-Threatening Newborn Condition
PPHN is a potentially life-threatening condition that affects a baby’s ability to get enough oxygen.
Before birth, babies receive oxygen through the placenta, not their lungs. Since their lungs are filled with fluid and not yet in use, the body naturally routes blood around them using temporary shortcuts in the circulatory system—the ductus arteriosus and the foramen ovale. After birth, when a baby starts breathing, these routes are supposed to close so blood can flow through the lungs and pick up oxygen. But with PPHN, that switch doesn’t happen properly. The lung vessels stay constricted and the bypass pathways remain open so blood skips the lungs and does not receive the oxygen the baby needs.
For Emily and JD the diagnosis was unexpected and terrifying. What had seemed like a healthy birth quickly became a fight to stabilize Estelle’s breathing and give her the best chance at recovery.
Doctors attempted treatments including CPAP and inhaled nitric oxide, a therapy used to relax the blood vessels in the lungs and improve oxygen flow. But even with these interventions, Estelle wasn’t responding.
“The next morning, they told us she needed a higher level of care and would need to be transferred,” Emily said.
Airlifted to Manning Family Children’s for Higher Level Care
Through a family connection, they arranged for Estelle to be airlifted to the neonatal intensive care unit (NICU) at Manning Family Children’s. The situation became critical almost immediately upon arrival.
When regular ventilation couldn’t keep Estelle’s oxygen levels stable, the NICU team acted fast. They put her on ECMO—short for extracorporeal membrane oxygenation—which is a highly advanced form of life support. It works like a heart-lung bypass, giving her tiny body a chance to rest and begin healing. 
“ECMO is typically used as a last resort when a baby’s heart or lungs are too weak to function on their own,” said Brian Barkemeyer, MD, a neonatologist involved in her care. “In Estelle’s case, her oxygen levels were dangerously low despite maximum support and ECMO gave her the best chance of survival.”
Estelle remained on ECMO for four and a half days. Once taken off ECMO, she was placed on nitric oxide and the NICU team gradually adjusted the levels until she no longer needed oxygen support. A team of neonatologists, respiratory therapists, and critical care nurses monitored her closely around the clock.
After being weaned off ECMO, Estelle’s pulmonary hypertension gradually began to improve. Still, the journey was far from over, and her medical team remained vigilant as new concerns emerged.
Digging Deeper: A Hidden Diagnosis
After her lungs stabilized, Estelle was still lethargic, wasn’t feeding well, and showed little progress. One of her providers suggested testing her cortisol levels, a key hormone regulated by the pituitary gland. The results showed very low levels in her body. An MRI revealed her pituitary gland was underdeveloped.
“The front portion of her pituitary gland didn't fully develop. After running a hormone panel, it was confirmed that she didn't have growth hormone or thyroid hormone along with the lack of cortisol,” Emily said. “That’s why she wasn’t feeding or responding like the team had hoped and extended our stay in the NICU for 71 days.” 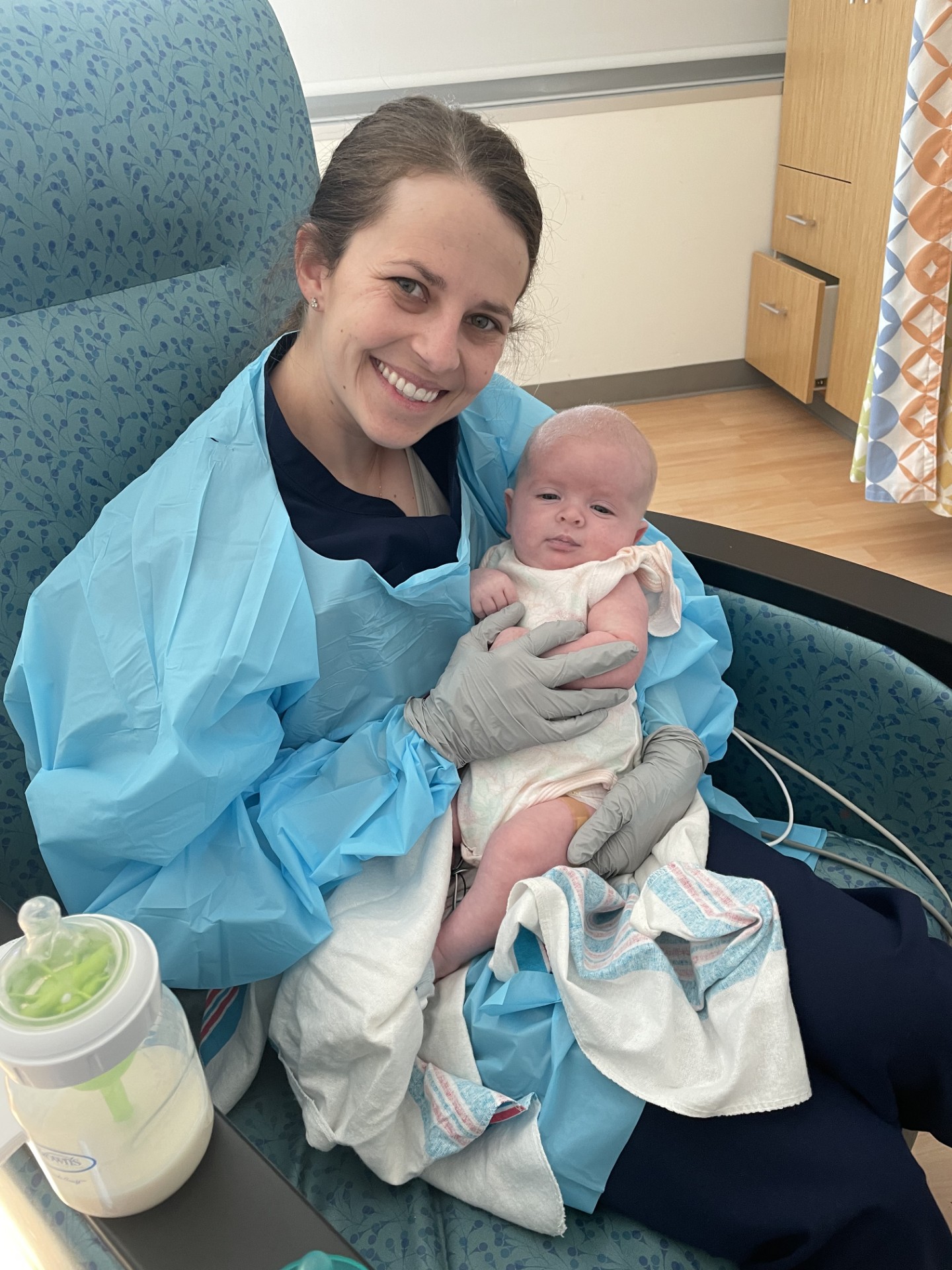
Estelle was diagnosed with panhypopituitarism, a rare condition where the pituitary gland doesn’t produce enough essential hormones. To better understand the cause, the medical team ordered genetic testing and ran a targeted panel based on her symptoms. The results showed that Estelle’s condition was genetic and more could be discovered with further testing as she matured.
One of the most concerning symptoms was Estelle’s difficulty feeding, likely caused by low cortisol and other hormones which help regulate appetite. She initially relied on a feeding tube—first oral, then nasal—but her intake remained too inconsistent for discharge.
“Some days she’d drink a bottle well; other days, she had no interest,” Emily recalled. Eventually, doctors placed a G-tube directly into her stomach to ensure consistent nutrition. Emily said the G-tube was what finally made it possible for them to go home instead of remaining in the hospital even longer.
71 Days in the NICU: Compassionate Care that Made A Difference
During Estelle’s 71-day stay in the NICU at Children’s, she made steady progress. She was weaned off oxygen and nitric oxide, began gaining weight, and started hitting key developmental milestones. Day by day, she fed better and grew stronger until finally, she was ready to go home.
“It was such a relief. We were ready to all be under one roof,” Emily said.
Looking back on their NICU journey, the Dunaways are filled with gratitude for the team at Children’s.
“It was amazing,” Emily said. “There were so many talented and compassionate caregivers—her doctors, nurses, therapists, even the cleaning staff. Everyone who came into Estelle’s room was kind and thoughtful. We built meaningful relationships and they cared for Estelle like she was their own. It made it easier to leave each day knowing she was in good hands.”
Through all the ups and downs, what sustained them most was their faith, knowing God was in control, and there was a talented team caring for their daughter.
“Initially we were in a state of shock,” Emily admits. “But my husband and I knew we needed to stay grounded in our faith. We had to trust the Lord and the care team. Whether it went the way we wanted or not, we had peace knowing that God was in control and took it day by day. Our family, friends and church community were a strong support system for us to continue to weather the storm.”
Life Today: Thriving at Home 
Today, Estelle, nicknamed Stella, is almost a year old and thriving. “She loves hanging out and laughing at her big sister,” Emily beams. “We’ve had the feeding tube removed. She’s babbling, growing, and just has this easygoing, happy personality with a touch of sass.”
Her follow-up care includes regular visits with her pediatrician, as well as ongoing appointments with Ricardo Gomez, MD, chief of Endocrinology at Children’s, who monitors her hormone levels and overall endocrine function to ensure healthy development. Because ECMO can impact both the heart and hearing, Estelle also sees cardiology and audiology specialists to make sure everything remains on track. In addition, she receives physical, occupational, and feeding therapies to support her continued growth and development.
With Estelle doing remarkably well, the Dunaways have even more to be thankful for as they anticipate the arrival of their third child this October.
“We’re just so grateful for everything—for our family, for the support we received, and especially for Estelle and the care she received,” Emily shared. “Seeing God heal her through the team at Manning Family Children’s has strengthened our faith and hope. We pray through Stella’s life, others can be encouraged in their situations and trust God in their struggle.”
For more information about the NICU at Manning Family Children’s, visit Neonatal Intensive Care | Manning Family Children's